GERD & Barrett’s Esophagus
In Barrett's esophagus, the tissue in the esophagus is replaced by tissue similar to the type of tissue normally found lining the intestines. This is a process known as intestinal metaplasia.
GERD & Barrett’s Esophagus
Although the symptoms of Barret’s esophagus alone are rare, a small population of people who develop this condition can also develop a rare type of cancer of the esophagus known as esophageal adenocarcinoma. Nearly affected 700,000 adults in the United States alone, Barrett’s esophagus is associated with gastroesophageal reflux disease or better known as GERD.
The exact causes of Barrett’s esophagus are yet to be determined, the same factors which cause GERD, resemble those that bring on Barrett’s. However, just because you are not experiencing heartburn does not mean you can’t have Barrett’s esophagus. Statistics show people with this condition have experienced heartburn three to five times more than those that didn’t.
Barrett’s esophagus diagnosis has an average age of diagnosis of 60, is uncommon in children but also not easy to determine the exact time the problem began. Being almost twice as common in men than women, along with much more occurrences in white men than men of other races.
Cancer of the Esophagus & Barrett’s Esophagus
Since Barrett’s esophagus does not cause any symptoms in itself, it’s even more imperative to treat as it seems to precede a particular kind of cancer known as esophageal adenocarcinoma. These risks of developing this cancer increase 30 to 125 times higher in patients with a history of Barrett’s esophagus. The rapid increase of this specific cancer in white men may be related to the increased numbers of obesity & GERD.
Diagnosing & Screening Barrett’s Esophagus
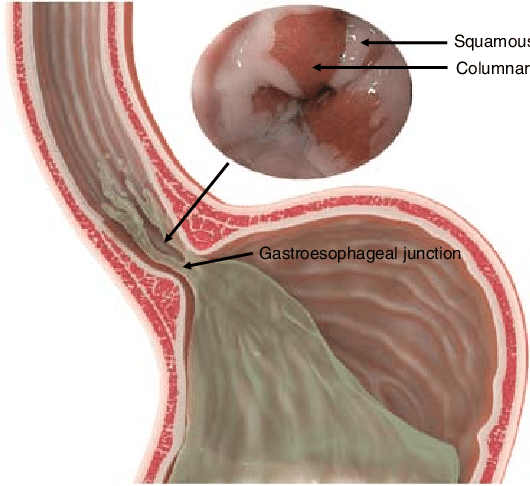
Barrett's esophagus with acid reflux. Inset: endoscopic view of metaplasia at the gastroesophageal junction.
Evaluation and Management of Premalignant Conditions of the Esophagus: A Systematic Survey of International Guidelines - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Barretts-esophagus-with-acid-reflux-Inset-endoscopic-view-of-metaplasia-at-the_fig1_335124101 [accessed 31 Mar, 2020]
An upper GI endoscopy is the only way to properly diagnose Barrett’s esophagus, by obtaining biopsies of the esophagus under visual examination. At this time there is no way to diagnose Barrett’s simply using symptoms, blood tests or even a physical examination.
During an upper GI endoscopic study, Dr. Michel Kahaleh guides a flexible tube equipped with a light and miniature camera also known as an endoscope down through the esophagus. During our visual examination if any tissue of the esophagus appears suspicious, we must obtain biopsies to property diagnose the reason behind these changes. A biopsy is simply the removal of relatively small pieces of tissue using devices internally through our endoscope. We have the most capable team of pathologists who then examine the tissue under microscopic guidance to confirm the diagnosis.
It is highly recommended that adults over the age of 40 with symptoms of GERD for years seek an endoscopic approach to determine if they have Barrett’s esophagus. If you have no symptoms of GERD we do not recommend screening for this condition.
Treatment of Barrett’s Esophagus
Unfortunately, with no cure for Barrett’s esophagus - patients who have esophageal cancer are usually recommended surgical intervention, until modern developments in advanced endoscopy have arrived.
Our treatment of Barrett’s esophagus is determined by the changes we see on a cellular level. When our pathologists examine the tissue obtained during biopsy they are able to determine how much dysplasia is seen in the cells. Dysplasia is the amount of changes prior to cancer being present - we grade these changes as low-grade or high-grade.
With no dysplasia being present, we treat symptoms of GERD with lifestyle changes and proper medications. We also recommend on-going upper GI exams for continued monitoring of the esophageal cells for any further changes in dysplasia. If no dysplasia was present upon initial examination, another endoscopy is repeated every three to five years.
Two potential options are available for those with low-grade dysplasia upon initial screening. One being a lifestyle & medicine change with repeat endoscopy in 1 years time. The second option is to endoscopically treat the esophageal area given the increased potential to develop esophageal cancer.
When diagnosed with high-grade dysplasia, the chance of developing esophageal cancer is much greater. Endoscopic intervention is highly recommended under these circumstances.
Endoscopic Therapies for Both Low & High-Grade Dysplasia
These therapies are all highly effective in the management of Barrett’s esophagus. It is a rare occurrence when traditional surgical intervention is required when the abnormal portion of the esophagus is taken and the remaining portion requires connection to the stomach.
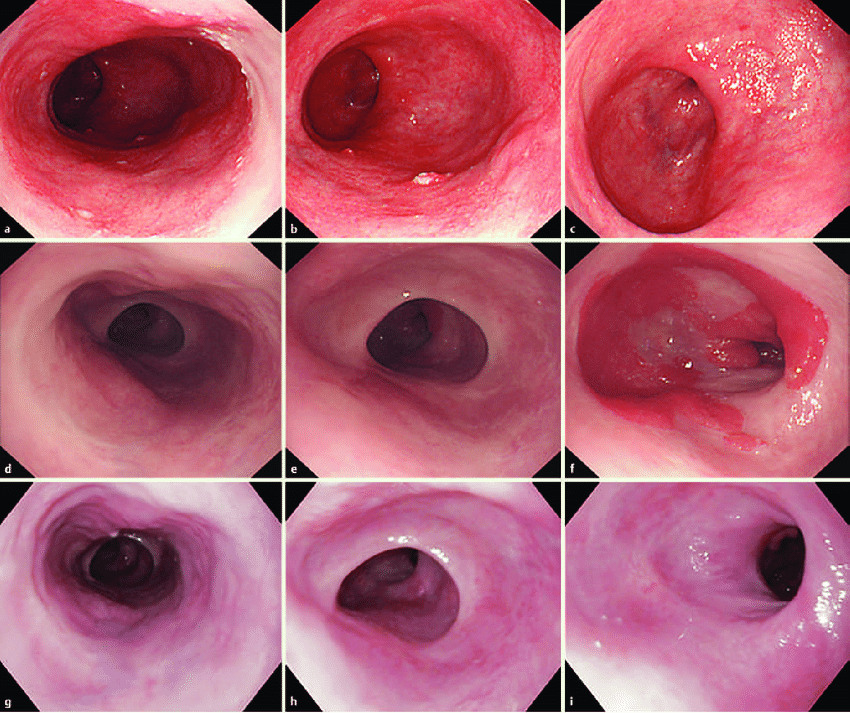
a Long-segment Barrett's esophagus (C4/M5). b A reddish and depressed lesion noted at the 7 o'clock position. c Rough surface and uneven redness observed. d, e Irregular structural and vascular patterns detected by magnifying endoscopy with narrow band imaging. f Endoscopic ultrasonography (20 MHz) showing the tumor in the mucosal layer with a normal submucosal layer (arrows)
Treatment of long-segment Barrett's adenocarcinoma by complete circular endoscopic submucosal dissection: A case report - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Endoscopic-findings-a-Long-segment-Barretts-esophagus-C4-M5-b-A-reddish-and_fig1_322606935 [accessed 31 Mar, 2020]
Endoscopic Resection
With the use of multiple devices which we pass through our endoscopes, we remove the abnormal cells entirely. This is achieved using two techniques which Dr. Kahaleh has spent years of his career perfecting:
- Endoscopic mucosal resection (EMR)
- Endoscopic submucosal dissection (ESD)
Cryotherapy
During this technique we are using cold liquid or gas to freeze the target damaged cells. This process involves freezing the cells, allowing time for them to thaw then freezing them once again. This cycle of freezing and thawing is what destroys this abnormal cells and allows them to be replaced with normal esophageal tissue once again. This procedure is approved by FDA and is extremely safe when correctly used.
Radiofrequency Ablation (RFA)
Similar to cryotherapy in that this is also an FDA-approved procedure. Unlike cryotherapy, during RFA we are using heat energy to destroy the abnormal cells. Similarly when the area undergoing ablation heals, those abnormal cells will be replaced by normal esophageal tissue. Normally this technique will require repeat sessions of RFA every 3 months until the damaged cells are fully removed.
Why Dr. Michel Kahaleh and his Team?
Dr. Michel Kahaleh has brought his extensive knowledge and passion to his new home in Hackensack, NJ. He uses the newest tools which have been shown to be more effective in detecting Barrett’s esophagus and establishing a diagnosis. With novel imaging techniques and the most innovative treatment modalities to treat his patients. Find Dr. Michel Kahaleh and make sure to use these tools and techniques to ensure the very best treatment and care for Barrett’s esophagus.